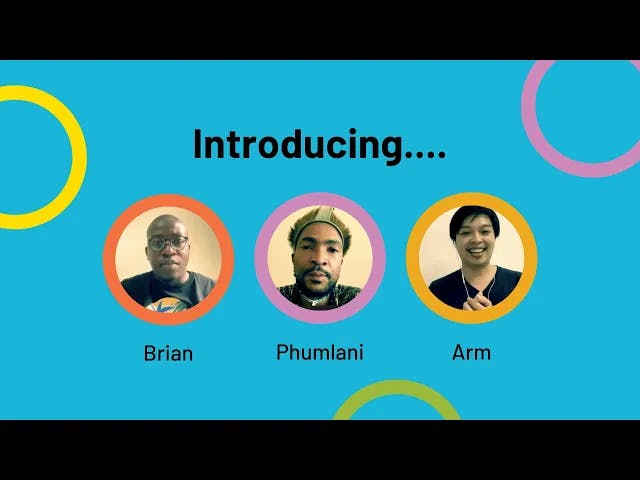
Brian is Director of LGBT rights organisation Uthingo Network and Phumlani is a sexual health activist, focusing on key populations and access to PrEP – both based in South Africa. Arm is a Campaign Officer based in Thailand for Apcom an LGBTQ+ organisation for Asia Pacific. Find out how they think healthcare workers can make HIV services more friendly for men who are more at risk of HIV than the general population.
What makes HIV services unfriendly?
Here are some of the biggest issues that prevent men who have sex with men seeking healthcare.
Some healthcare workers can be unfriendly, judgemental or even hostile about their patients’ sexual orientation.
Brian says: “I think the biggest barrier is the negative perceptions and attitudes by healthcare professionals. Their personal, religious or cultural ideas and beliefs that stigmatise gay men.”
Phumlani says: “A lot of people just shy away from services because of the stigma they face. So an example would be an MSM individual being categorised and being boxed up and being made to choose, you know, like are you gay or bisexual, for example?”
If healthcare workers don’t keep their patient’s personal information and circumstances private and confidential, it can have a devastating impact on their client’s lives. The fear of having their confidentiality breached can prevent people seeking the healthcare they need.
Arm says: “I have my friend that worked as like a sex worker or in the porn industry. Some of their data was leaked in social media, when they went to a healthcare service, and they avoided to use the service and found other ways to get tested or to get PrEP.”
Men who have sex with men (MSM) have specific health needs. When healthcare workers aren’t trained in these, they can’t provide good services.
Brian says: “Sometimes you find healthcare providers who are well meaning, but because they don't have that information or training, they can’t adequately provide services to MSM.”
It’s also important that healthcare workers see their clients as individuals and don’t make assumptions based on their sexual orientation or activity.
Phumlani says: “We [men who have sex with men] don't all have the same experience and we don't all have the same lifestyle.”
How can HIV services be more welcoming?
When HIV services are friendly, more men who have sex with men will come. Here are some ways to improve your service.
Even if people are well-meaning, ignorance can cause discrimination. Arrange for training to help you and other healthcare workers understand and be more aware of the needs and feelings of men who have sex with men.
Brian says: “Sensitisation training for healthcare workers helps them to understand different identities. We found healthcare providers tend to view their patients from a cisgender heterosexual outlook. But as soon as they get education, there is a mind shift. It’s about learning to provide services irrespective of people's identities and treating all patients with respect.”
Phumlani says: “Go out and do research and have conversations with various MSM groups where you actually get to understand our lived experiences.”
Allow patients to self-screen on a form so they don’t need to speak out loud about their sexual orientation or health concern in a busy clinic.
Brian says: “I worked on a research project with MSM and some individuals asked for a self-screening questionnaire, which you take to a healthcare provider. So by the time they sit down with you, they know exactly what's happening without having to speak out loud or embarrass you in front of other patients.”
Peer educators or health provider champions can speak to men who have sex with men in their communities and refer clients to your clinic.
Arm says: “We go to the nightclub and distribute to people, or we let them fill in an online survey and then distribute it to them – we call it a safe-play pack, it's 15 condoms and 15 lubricants for each month! This activity has become well-known through our work. We did it online so people can access prevention tools conveniently and for free.”
How can service facilities be made more accessible?
The way facilities are set up can sometimes bring barriers for men who have sex with men, diversifying the way services are offered can help increase access.
An HIV-self test allows someone to test for HIV in privacy instead of in a clinic. Hand out HIV self-tests in your clinic to encourage people to test.
We know that coming to a clinic can cause stress. Offer home delivery or delivery in the community to limit the number of times men who have sex with men have to come to the clinic to collect ARVs or PrEP, to help them adhere to their treatment.
Brian says: “Delivery of medication would actually be a big win for people.”
Phumlani says: “During COVID-19 they would come in the mobile clinics to give you PrEP. They would call you and ask you where you are. Let's meet at a particular garage or let's meet at a particular spot. You get tested. Draw your bloods, they give you PrEP and then they call you back.”
Clinics that specialise in healthcare for men who have sex with men can be a good way to provide a safe space.
Brian says: “I’d rather go to a space where I know that I don't have to explain myself because the clinic understands my needs.”
However, ultimately all clinics should be spaces where men who have sex with men feel safe and understood.
Because of stigma, often people don’t want to be seen visiting a clinic.
Arm says: “Many things stop men coming to get this service. The first one is the area or the place of the clinic. Some of the clinics are close to the university, some of the clinics are close to the workplace and maybe if I'm a gay man, I don’t want anybody to know I have to get the service to check my blood at the clinic or to get PrEP.”
Open the clinic after work hours to enable more men who have sex with men to come without explaining where they are going to their lecturer or employer.
Phumlani says: “Let's say they open from 5pm until 9pm to allow other people to come in, it would definitely help.”
Arm says: “Give us more information like what is the next process after this. Because some clinics they won't give us more detail. In their opinion, if they give us more detail maybe the MSM that use that clinic will move to another one. But this thought is not quite right, because if you give them the way to get easy access to the service it will be good for the person who used the service. Not just you give me only this information and next time just come back to the same clinic again. The same clinic again all the time."
Work with other community clinics to link up and allow people to be referred and visit different clinics when it suits them.
Arm says: “Make us confident that the data will be stored correctly and be safe and not leaking. Because in Thailand the data are leaking quite often, as I see in Twitter all the time.”
Arm says: “It would be good if the clinic would have a one-stop service to check everything, like HIV along with hepatitis C and other STIs together. It will save time and cost. We don't need to get to the clinic and then make another appointment to another clinic.
“And another thing for a person like me, who doesn’t want to go to the clinic or other MSM that don't want to visit the services, is teleconsultations – that would help a lot.”
Examples of poor treatment at HIV services
These are examples of when men who have sex with men have been treated poorly at HIV services. By hearing the personal experiences of men in this group, you can learn how to improve your services. We are protecting these individuals’ privacy by keeping the quotes anonymous.
“I went to a clinic to have an anal STI treated. The nurse went out of their way to embarrass me by speaking so loudly that everyone in the corridors and other consultation rooms could hear.”
“A healthcare provider called the other staff members into the consultation room, saying ‘come and see this’, treating me with no privacy at all.”
“I told the nurse that I am gay and she offered to pray for me to convert me from being gay to being straight. It made me feel terrible and completely unaccepted for who I am.”
“I knew that staff from the local clinic for men who have sex with men would gossip about their patients in social circles. It stopped me going to get the treatment I needed, I was too scared.”
“I went to get PrEP and the replacement nurse started asking me questions about my religious views, my lifestyle and what does my family think of me. I found that very inappropriate. She should have been asking me about when last did you get tested? When last did you have sexual intercourse? Was it anal sex? You know, like those kind of questions, so that she's able to provide proper services.”
“I was misgendered by a health worker – it’s not a nice feeling when they assume you are a woman and in fact you’re a man – or the other way around. Health workers shouldn’t make assumptions about your gender they should ask whether you use he or she to describe yourself – this should be included on a screening form.”
Do you know of any resources to help healthcare workers make HIV services more friendly to men who have sex with men? Let us know by getting in touch at: info@beintheknow.org.